Stroke Volume Equation: A Critical Component of Cardiovascular Physiology
Stroke Volume Equation: A Critical Component of Cardiovascular Physiology
The human cardiovascular system is an intricate network of vessels and pumps that ensures a continuous supply of oxygen and nutrients to tissues while removing metabolic wastes. At the heart of this system is the heart itself, which beats approximately 100,000 times a day, pumping blood through the body. One key measurement that gives insight into the heart’s function is stroke volume—the amount of blood the heart ejects with each beat. Understanding the stroke volume equation is critical for both clinicians and physiologists, as it plays a central role in determining cardiac output and overall cardiovascular health. This article will explore what stroke volume is, the equation used to calculate it, and its importance in medical diagnostics and treatment.
Understanding Stroke Volume
Before diving into the equation itself, it’s essential to understand what stroke volume represents. Stroke volume (SV) is the amount of blood pumped by the left ventricle of the heart during each contraction or heartbeat. This measurement is important because it reflects the heart’s ability to meet the body’s circulatory demands. Typically, the average stroke volume for a healthy adult is about 70 mL per beat, though this can vary depending on factors such as age, fitness level, and medical conditions.
Stroke volume is a crucial component of cardiac output, which is the total volume of blood the heart pumps per minute. Cardiac output (CO) is the product of stroke volume (SV) and heart rate (HR), expressed in the following equation:
CO = SV × HR
Thus, stroke volume is an essential determinant of overall cardiovascular function. Any changes in stroke volume, whether due to disease, exercise, or other factors, will directly influence cardiac output and, in turn, the amount of oxygen and nutrients delivered to the body’s tissues.
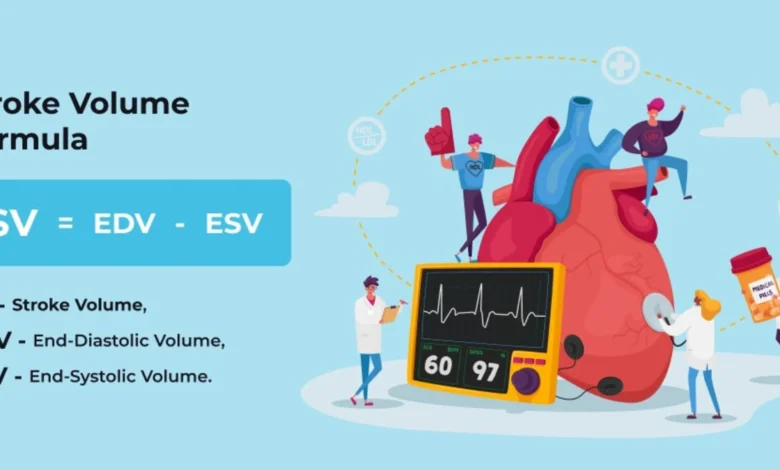
The Stroke Volume Equation
The stroke volume equation allows clinicians and researchers to quantify the amount of blood ejected from the heart during each contraction. The basic equation to calculate stroke volume is:
SV = EDV – ESV
Where:
SV = Stroke Volume (mL)
EDV = End-Diastolic Volume (mL) – the volume of blood in the ventricle at the end of diastole (just before contraction).
ESV = End-Systolic Volume (mL) – the volume of blood remaining in the ventricle at the end of systole (just after contraction).
Breaking Down the Equation
End-Diastolic Volume (EDV):
The EDV is the total amount of blood present in the ventricle at the end of diastole, which is the relaxation phase of the cardiac cycle. During diastole, the heart’s ventricles fill with blood returning from the body and lungs. The amount of blood entering the ventricles depends on several factors, including venous return (the flow of blood back to the heart), the compliance of the ventricular walls, and the time available for filling (which can be affected by heart rate). A higher EDV generally means a higher stroke volume because more blood is available to be pumped out with each contraction.
End-Systolic Volume (ESV):
ESV is the volume of blood remaining in the ventricle after the heart has contracted and ejected blood into the aorta. Several factors influence ESV, including the contractility of the heart muscle and the resistance the heart has to overcome to pump blood (known as afterload). A lower ESV indicates that the heart is more efficient at ejecting blood, resulting in a higher stroke volume.
Stroke Volume (SV):
By subtracting the ESV from the EDV, the stroke volume equation calculates the amount of blood the heart pumps with each beat. For example, if the EDV is 120 mL and the ESV is 50 mL, the stroke volume would be:
SV = 120 mL – 50 mL = 70 mL
This result reflects the efficiency of the heart’s ability to pump blood and meet the body’s circulatory demands.
Factors Influencing Stroke Volume
Several physiological and pathological factors influence stroke volume, making it a dynamic variable that changes in response to the body’s needs. Some of the key factors include:
Preload:
Preload refers to the amount of stretch the ventricular muscle fibers experience during filling, which is influenced by the volume of blood returning to the heart. Increased preload typically leads to an increase in stroke volume, as per the Frank-Starling law of the heart, which states that the greater the stretch of the ventricular muscle, the stronger the subsequent contraction.
Afterload:
Afterload is the resistance the ventricles must overcome to eject blood into the aorta and pulmonary artery. High afterload, such as in conditions like hypertension, increases the workload on the heart and can reduce stroke volume. Conversely, lower afterload makes it easier for the heart to pump blood, increasing stroke volume.
Contractility:
Contractility refers to the intrinsic ability of the heart muscle to contract independently of preload and afterload. An increase in contractility, often influenced by sympathetic nervous system stimulation or medications like inotropes, boosts stroke volume by reducing the ESV. Decreased contractility, on the other hand, reduces stroke volume.
Heart Rate:
Heart rate can indirectly influence stroke volume. A higher heart rate, for example, shortens the diastolic filling time, potentially reducing EDV and, in turn, stroke volume. However, during exercise, the body compensates for a higher heart rate with increased venous return and stronger contractions, maintaining or even increasing stroke volume.
Clinical Relevance of Stroke Volume
Accurately measuring stroke volume is essential in both clinical and research settings. In conditions like heart failure, where the heart’s ability to pump efficiently is compromised, stroke volume is often reduced. Clinicians use various diagnostic tools, such as echocardiography and cardiac catheterization, to assess stroke volume and guide treatment decisions.
In athletic performance, stroke volume also plays a significant role. Well-trained athletes often have larger stroke volumes, enabling their hearts to pump more blood with each beat, which is a key factor in endurance performance. This adaptation allows them to maintain high levels of oxygen delivery to muscles during prolonged physical activity.
Moreover, stroke volume can be a key parameter in managing patients undergoing surgery or those in critical care settings. Monitoring stroke volume helps in assessing fluid status, cardiac function, and response to therapeutic interventions such as intravenous fluids or medications that affect the heart’s contractility and vascular resistance.
Conclusion
The stroke volume equation—SV = EDV – ESV—provides valuable insight into the heart’s function and efficiency. Understanding how stroke volume is calculated and influenced by various physiological factors is crucial for diagnosing and managing cardiovascular conditions. Whether in athletic performance, clinical diagnostics, or critical care, stroke volume serves as a fundamental measure of the heart’s ability to meet the demands of the body. As cardiovascular research advances, the stroke volume equation will continue to be a key tool in optimizing heart health and improving patient outcomes.
You Can More Read
India National Cricket Team vs West Indies Cricket Team Timeline: Evolution of a Cricketing Battle